About
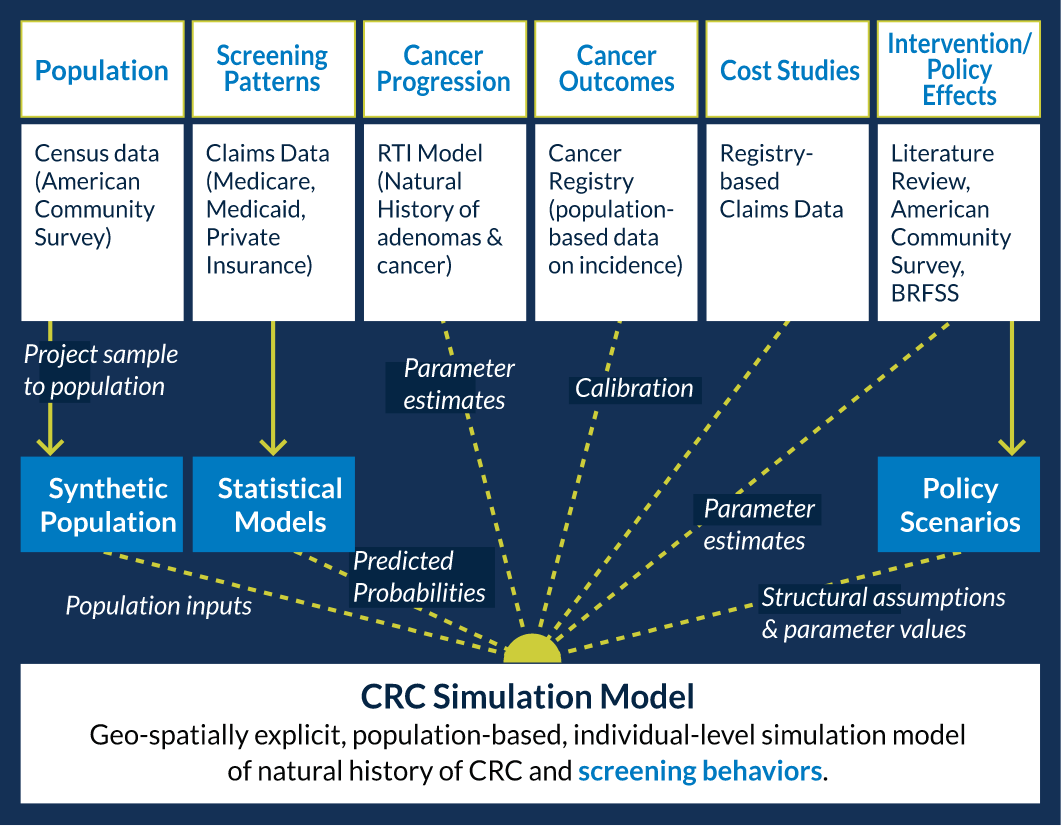
We use population-level models that create a real-world simulated cohort of individuals living in a particular state, with features like age, sex, race/ethnicity, and insurance status that resemble the Census for that state. These models are capable of predicting the short- and long-term health outcomes (for example, likelihood of developing colorectal cancer) and associated costs of current standards of care (for example, the expected cost of treating colorectal cancer), and how these outcomes are expected to change over time as a result of specific healthcare interventions and policies. This approach allows for estimating and comparing the differential costs and health impacts of strategies intended to improve population health outcomes.
Our models are currently designed to simulate colorectal cancer-related outcomes within the state populations in North Carolina and Oregon, as well as subgroups within these states (for example, African Americans or Medicaid-insured people). We can estimate the impact of implementing evidence-based interventions (for example, mailing a stool kit to age-eligible individuals who are overdue for colorectal cancer screening) or health policy changes (e.g. insurance expansion) on cancer screening, cancer occurrence, cancer death, and related costs for these populations. Right now, we focus on estimating how specific interventions and policies of interest to decision makers will affect the percentage of age-eligible individuals up-to-date with colorectal cancer screening, the number of cancer cases prevented, and total costs of cancer screening, cancer diagnosis, and cancer treatment, compared to current standards of care (i.e., status quo).